Respiratory Muscle Function and Outcomes following SCI
The higher the level of motor complete SCI, the greater the
- impact on respiratory function
- risk for secondary complications
- indication for ventilation support
Any acute injury above the level of T12 neurological level of SCI will result in some respiratory dysfunction: there is often respiratory muscle (abdominal, intercostal and diaphragm muscles) weakness and/or paralysis, which is initially a flaccid paralysis due to spinal shock. Compliance changes to the lung and chest wall also develop. This often results in paradoxical breathing patterns and the work of breathing increases, with the additional recruitment of accessory muscles necessary.
The impact of changes to the sympathetic nervous system should also be considered in combination with respiratory muscle paralysis.
If the SCI is above T6, there is also an additional autonomic dysfunction with the loss of sympathetic nervous system control and predominance of parasympathetic nervous system activity. This further impacts lung volumes and airway clearance and results in:
- decreased pulmonary surfactant production
- increased pulmonary secretion production
- airway bronchospasm
Assessment of respiratory muscle activity can be informed using a review of breathing patterns, coughing effectiveness and spirometry.
Respiratory Muscles and Function
Respiration is a combination of inspiration and expiration, according to physiological and functional needs. Inspiration involves primarily the diaphragm and the intercostal muscles. Other accessory muscles can be recruited to increase volume, rate or the force generated.
Expiration is a passive process which occurs when the diaphragm relaxes inducing the elastic recoil of the lungs and chest wall.
However, forced expiration to speak, sing, huff or cough primarily requires activation of the abdominal muscles, co-ordinated with glottal function. Again, other accessory muscles can be recruited as needed, especially to cough.
NOTE:
- Respiratory muscles often work synergistically together, including antagonists for respiratory function eg.cough
- Respiratory muscles often have other functional roles beyond respiration
- Many respiratory muscles are small and prone to fatigue: although a larger muscle with a variety of muscle fibre types, the diaphragm is also prone to fatigue if breathing mechanics are significantly altered due to neurological dysfunction
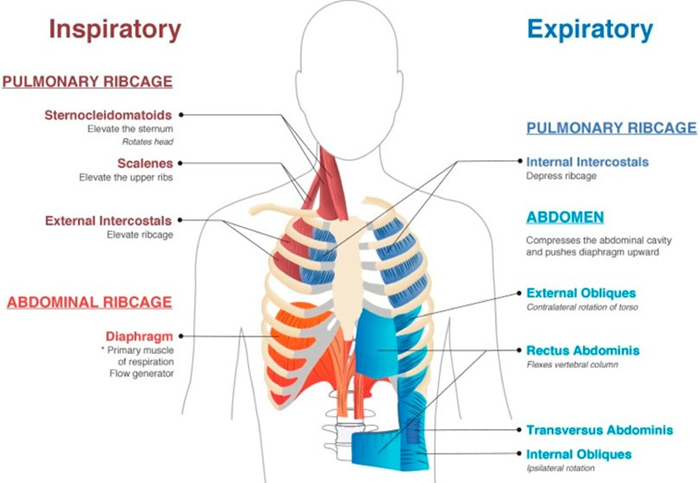
Muscles of Respiration
Source: https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2022.838414/full
Primary Respiratory Muscles
INSPIRATION
DIAPHRAGM
Innervation: Phrenic nerve C3-5
Respiratory roles and commments:
Quiet Inspiration, Forced Inspiration
In addition to full innervation, optimal diaphragm contractile efficiency depends on the stabilising alignment provided by the:
1. abdominal muscles (position the abdominal contents against the diaphragm to optimise its “dome” shape for contraction, especially in sitting)
2. intercostal and other deep thoracic muscles (stabilise the rib cage/intercostal spaces during changes in intrathoracic pressures during diaphragm contraction and relaxation)
In an acute SCI, the initial flaccid paralysis of the abdominal and intercostal muscles often results in paradoxical breathing patterns and an increase in the work of breathing, especially in sitting.
As spinal shock resolves a spastic paralysis of the intercostals +/- abdominal muscles may improve breathing patterns.
Use of abdominal binders in sitting can assist positioning of the diaphragm for enhanced contractile efficiency, improving lung volumes for ventilation, cough and speech.
Other functions & comments:
Generation of transdiaphragmatic pressure: by co-contracting with upper airway/larynx/tongue and pelvic floor muscles and relevant sphincters for expulsive or sustained expiration eg. cough, speech etc but also general postural stability when upright
Establishment of an anti-reflux mechanism: by the crural component of the diaphragm supporting the functioning of the lower esophageal sphincter
EXPIRATION
ABDOMINALS: RECTUS, EXTERNAL OBLIQUE, INTERNAL OBLIQUE, TRANSVERSUS
Innervation: Spinal nerves T7-12
Respiratory roles and commments:
Forced Expiration, Cough
Other functions & comments:
Assist diaphragm positioning to optimize inspiratory volumes, especially in sitting
Generate transabdominal pressure to support venous return, aid voice projection, assist bladder and bowel emptying, maintain postural stability when the trunk is under load/exertion
Initiate active posterior pelvic tilt or trunk flexion for movement, as well as static and dynamic postural reactions
STABILISING and ACCESSORY MUSCLES
INTERCOSTALS: EXTERNAL and INTERNAL
Innervation: Spinal nerves T7-12
Respiratory roles and commments:
Quiet Inspiration, Forced Inspiration, Forced Expiration, Cough
Inspiration and forced expiration: changing the volume of the thoracic cavity
Other functions & comments:
Stabilise the rib cage/intercostal spaces during changes in intrathoracic pressures, especially to counteract the descent of the diaphragm during inspiration and the relaxation of the diaphragm during expiration
Other deep thoracic muscles that support the intercostal muscle function include: innermost intercostal muscles, subcostalis, and transversus thoracis.
OTHER MUSCLES
SCALENES Spinal Nerves 3-8
STERNOCLEIDOMASTOID Accessory Cranial Nerve XI and C1,2
UPPER TRAPEZIUS Accessory Cranial Nerve XI
SERRATUS ANTERIOR Long Thoracic Nerve of Brachial Plexus C5-7
PECTORALIS MAJOR and MINOR Lateral/Medial Pectoral Nerves of Brachial Plexus C5-T1
LATISSIMUS DORSI Thoracodorsal Nerve C6-8
Respiratory roles and commments:
Forced Inspiration, Forced Expiration, Cough
Inspiration and forced expiration: changing the volume of the thoracic cavity via action of reversed origin and insertion, improved by positioning the upper limb in a closed kinetic chain
Other functions & comments:
Head, neck, scapular and upper limb primary movement and stabilisation
Level of SCI and Respiratory Outcomes
The ventilation outcomes and respiratory needs listed below have a direct correlation to the degree of respiratory muscle paralysis. The impact of changes to the autonomic nervous system (ANS) should also be considered in combination with respiratory muscle paralysis.
| Neurological level | Respiratory Muscle and ANS Dysfunction | Ventilation Outcomes and Respiratory Needs |
| C1-C3 | Full to severe diaphragm paralysis Full abdominal and intercostal muscle paralysis Accessory muscle paralysis except for sternocleidomastoid and upper trapezius Impaired ANS function affecting cardiovascular (CV) and respiratory system | Full time ventilation support via ventilator +tracheostomy Bronchial hygiene and respiratory prophylaxis cares: secretion management, pulmonary and chest wall compliance maintenance Abdominal binder if tolerated Cough augmentation device +/- manual assisted cough Voice and speech generation needs |
| C3-C4 | Severe to partial diaphragm paralysis Full abdominal and intercostal muscle paralysis Accessory muscle paralysis except for sternocleidomastoid, upper trapezius and weak portion of scalenes Impaired ANS function affecting CV and respiratory system | Full time ventilation support via ventilator +tracheostomy OR face/mouth non-invasive ventilation (NIV) Periods of unassisted ventilation (ventilator free time) may be possible through the day; ventilation over night during sleep likely required Abdominal binder if tolerated Bronchial hygiene and respiratory prophylaxis cares: secretion management, pulmonary and chest wall compliance maintenance, inspiratory muscle training (IMT) Cough augmentation device +/- manual assisted cough Voice and speech generation needs Sleep disordered breathing risk for assessment and management |
| C4-C5 | Partial to no diaphragm paralysis Full abdominal and intercostal muscle paralysis Accessory muscle paralysis except for sternocleidomastoid, upper trapezius and some scalene activity Impaired ANS function affecting CV and respiratory system | Full time ventilation initially May be slow to wean to independent breathing- especially in sitting May benefit from face/mouth non-invasive ventilation (NIV) over night or when unwell Abdominal binder if tolerated Bronchial hygiene and respiratory prophylaxis cares: secretion management, pulmonary and chest wall compliance maintenance, inspiratory muscle training (IMT) Cough augmentation device +/- manual assisted cough Voice and speech generation managed with physical strategies eg. abdominal binder and accessory muscles Sleep disordered breathing risk for assessment and management |
| C6-C8 | No diaphragm paralysis Full abdominal and intercostal muscle paralysis Increasing availability of accessory muscles, including full scalene activity May have some weak portion of serratus anterior, pectoralis major activity and latissimus dorsi activity Impaired ANS function affecting CV and respiratory system | May benefit from face/mouth non-invasive ventilation (NIV) when unwell Abdominal binder if tolerated Bronchial hygiene and respiratory prophylaxis cares: secretion management, pulmonary and chest wall compliance maintenance, inspiratory muscle training (IMT) Cough augmentation device +/- manual assisted cough Voice and speech generation managed with physical strategies eg. abdominal binder and accessory muscles Sleep disordered breathing risk for assessment and management |
| T1-T4 | No diaphragm paralysis Full abdominal and lower intercostal muscle paralysis Some upper intercostal availability Full availability of accessory muscles, except for some deep thoracic and paraspinal muscles Improving ANS function affecting CV and respiratory system | Independent breathing May benefit from face/mouth non-invasive ventilation (NIV) when unwell Abdominal binder if tolerated Bronchial hygiene and respiratory prophylaxis cares: secretion management, pulmonary and chest wall compliance maintenance, inspiratory muscle training (IMT) Manual assisted cough or cough augmentation device Voice and speech generation managed with physical strategies eg. abdominal binder and accessory muscles Sleep disordered breathing risk for assessment and management |
| T5-T12 | No diaphragm paralysis Improving intercostal and then abdominal muscle activity Full availability of most accessory muscles, except for reduced deep thoracic and paraspinal muscles Minimal disruption to ANS affecting CV and respiratory system below T6. | Independent breathing May benefit from face/mouth non-invasive ventilation (NIV) when unwell Abdominal binder if needed Bronchial hygiene and respiratory prophylaxis cares: secretion management, pulmonary and chest wall compliance maintenance, inspiratory and abdominal muscle training (IMT) Manual assisted cough or cough augmentation device if needed Voice and speech generation normalising Sleep disordered breathing risk may require assessment and management |
| L1 and Below | Nil respiratory muscle paralysis Normal ANS control of CV and respiratory system | Independent breathing, normal cough Nil respiratory function changes except for loss of pelvic floor control assisting intra-abdominal pressure generation Voice and speech generation normal Nil SCI related sleep disordered breathing risk |
Adapted from Source: Berlowitz DJ, Wadsworth B, Ross J. Respiratory problems and management in people with spinal cord injury. Breathe 2016; 12: 328–340.
References
Berlowitz DJ, Wadsworth B, Ross J. Respiratory problems and management in people with spinal cord injury. Breathe 2016; 12: 328–340.
Mullen, E., Faltynek, P., Mirkowski, M., Benton, B., McIntyre, A., Vu, V & Teasall, R. (2022) Acute Respiratory Management Following Spinal Cord Injury. In: In: Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Noonan VK, Loh E, Sproule S, McIntyre A, Querée M, editors. Spinal Cord Injury Rehabilitation Evidence. Version 6.0. Vancouver: p. 1-51. acute-respiratory_V7.pdf (scireproject.com)
Bitnar, P. Hlava, S. Štovíček, J & Kobesová, A. (2018) Diaphragm in the role of esophageal sphincter and possibilities of treatment of esophageal reflux disease using physiotherapeutic procedures European Respiratory Journal, 52 (suppl 62) PA2446; DOI: 10.1183/13993003.congress-2018.PA2446
Respiratory Management in Spinal Cord Injury – Physiopedia (physio-pedia.com)
Sheel AW, Welch JF, Townson AF (2018). Respiratory Management Following Spinal Cord Injury. In: Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Noonan VK, Loh E, Sproule S, McIntyre A, Querée M, editors. Spinal Cord Injury Rehabilitation Evidence. Version 6.0. Vancouver: p. 1-72. Microsoft Word – FINAL Resp V6 Chapter May 30 2018.docx (scireproject.com)
Tang A, Bordoni B. Anatomy, Thorax, Muscles. [Updated 2023 Jul 24]. Treasure Island (FL): StatPearls Publishing; 2024 Jan https://www.ncbi.nlm.nih.gov/books/NBK538321/
Terson de Paleville DG, McKay WB, Folz RJ, Ovechkin AV. (2011) Respiratory motor control disrupted by spinal cord injury: mechanisms, evaluation, and restoration. Transl Stroke Res 1;2(4):463-73. Respiratory Motor Control Disrupted by Spinal Cord Injury: Mechanisms, Evaluation, and Restoration – PMC (nih.gov)