Assessment of Respiratory Function
The goal of a comprehensive respiratory function assessment is to
- provide a baseline respiratory assessment
- inform early management planning and intervention
- monitor for potential deterioration, especially in the acute management of SCI
Clinical Assessment
Clinical assessment should be completed by the MDT. It will be more intensive following an acute, above T12 neurological level of SCI and for people with chronic SCI who become acutely unwell.
The best position to assess respiratory function is supine. This position reduces the work of breathing and allows observation of the individual’s breathing pattern. However, any risk of aspiration in full supine must be considered and managed accordingly.
Signs of deterioration:
- drowsiness and lack of concentration
- slurring of speech
- decreased ability to co-operate with coughing
- worsening O2 and CO2 blood gases
- altered respiratory rate
- decline in respiratory function tests
- decreased air entry on auscultation
- increased production of sputum and /or change in colour
Resolution and improvement:
Respiratory function improves early post SCI when there is:
- reduction and resolution of inflammation and oedema around the spinal cord site of injury
- improvement in diaphragm function and accessory neck muscle recruitment in conjunction with resolving spinal shock: increasing rib cage stability and correcting paradoxical breathing patterns
This results in improved respiratory function tests with significant increases in vital capacity within 5 weeks of injury and approximate doubling of vital capacity within 3 months.
Observation
General Observations
Observations such as
- oxygen saturations and respiratory rate (direct correlation to respiratory muscle function)
- hypotension, hypothermia or bradycardia (secondary to the sympathetic nervous system impairment)
- increased temperature (may be indicative of a respiratory infection or pulmonary embolism)
Breathing Pattern
Observation of the breathing pattern is important to establish a baseline for the individual and will be directly impacted by the degree of impairment of the respiratory muscles. Breathing pattern changes will continue to develop if there is further ascension of SCI lesion level secondary to spinal cord bleeding and oedema. Assessment of breathing pattern should be reviewed repeatedly during the acute phase.
Observational assessment of the quality of the movement of the breathing pattern involves assessing any deviation from the normal abdominal versus thoracic pattern of inspiration which occurs synchronously:
- abdominal rise (then fall during passive expiration)
- lateral lower rib expansion
- rib cage anterior/posterior movement elevation
Observational assessment of the quality of the movement of the breathing pattern is best assessed with the patient positioned supine. Observe quiet and deep inspiration, from the:
- foot end of the bed to determine the symmetry of diaphragm descent into the abdomen
- each side of the bed to determine the abdominal versus thoracic pattern of movement
Paradoxical Breathing Pattern
For individuals with an acute, above T12 neurological level of SCI resulting in paralysis of the abdominal, intercostal and possibly diaphragm muscles, the work of breathing is increased. This is compounded in the acute phase when spinal shock is present, resulting in not only paralysis but flaccidity of muscles, especially the intercostal muscles. A paradoxical breathing pattern commonly develops and further increases the work of breathing.
What typically occurs during inspiration, is that any abdominal rise, results in an inward drawing of the ribcage in response to the increased negative intrathoracic pressure generated.
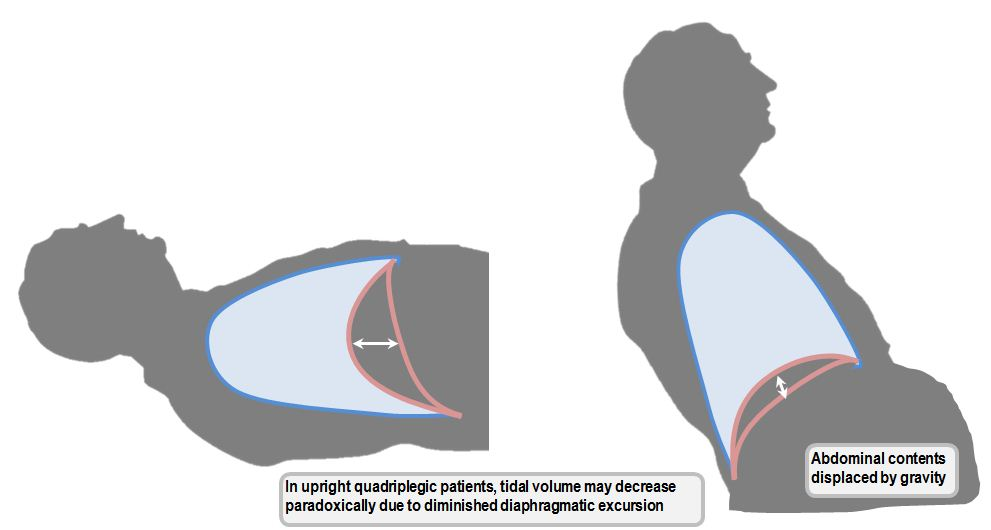
Work of Breathing: Supine vs Sitting
Finally, the overall work of breathing +/- speech is also assessed. Significant accessory muscle recruitment, in the presence of paradoxical breathing and other signs eg. increased respiratory rate, indicates increased work of breathing. It is a sign of respiratory distress that will progress to respiratory fatigue and even respiratory failure if not addressed promptly with positioning and support ventilation strategies.
The optimal positioning for improved breathing after acute SCI is supine, although this may need to be reconsidered in the presence of a large abdomen (distention, obesity) and chronic SCI.
There is a strong recommendation that positioning in supine should be provided (in favour of sitting) to improve lung volumes in people with acute SCI who have abdominal muscle paralysis or weakness.
In comparison to supine, positioning an individual with an acute, above T12 neurological level of SCI in upright sitting will most likely increase the work of breathing. As described above, the loss of abdominal muscle function optimising the “domed” starting position of the diaphragm via the abdominal contents, is further exacerbated. The diaphragm “sags” even more and the work of breathing can increase significantly.
Not only should the impact of abdominal muscle paralysis on diaphragm be considered, but any major abdominal resection surgery related to associated injuries. This loss of abdominal content “bulk” will also impact the “domed” start position of the diaphragm for ventilation, and especially in sitting.
Once medically stable, mobilising in sitting should only occur once the work of breathing in supine has been addressed with adequate ventilatory supports/strategies and preferably as spinal shock resolves. Mobilising in sitting requires adequate Multidisciplinary Team planning and suitable equipment/supports for success.
In the presence of reduced or absent abdominal muscle function, use of a fitted abdominal binder may assist improvement of diaphragm positioning in sitting and increase lung volumes.
Resources
Quality and Effectiveness of Cough
The degree of respiratory muscle impairment not only impacts the quality and effectiveness of inspiration, but also forced expiration.
While quiet expiration is a passive process, forced expiration including cough and huff, requires forceful abdominal muscle contraction following a large inspiratory breath.
Assessment of quality and effectiveness of a cough and huff is required to identify if other strategies for secretion clearance and ventilation should be implemented.
Any risk of aspiration including saliva, as well as emergencies such as choking should also be determined.
Observe
- force of cough: rate the loudness/likely effectiveness of cough or huff generated either spontaneously or on command
- productivity: determine if the cough productive or dry and describe sputum colour, thickness and amount
Swallow, Voice and Speech
There can be swallow function changes following prolonged intubation and/or anterior cervical discectomy and fusion (ACDF).
Any increased risk of aspiration including saliva, poor pharyngeal clearance and pain on swallowing should be noted.
It is highly recommended to complete an early swallow and voice assessment post extubation/ACDF.
Voice and phonation/speech can also vary depending on completeness and level of injury due to the impact on lung volumes, forced expiration, diaphragm function and subglottal pressure.
Changes to voice and phonation/speech will also be indicative of respiratory dysfunction
- shorter maximum phonation time
- higher degree of phonatory instability
- limited number of syllables per breath
- lower speech rate
- reduced volume
- change in quality of speech such as breathiness and roughness
- voice changes in setting of possible vocal cord dysfunction
Physical assessment of respiratory function
Auscultation and Palpation
Lung Sounds
Auscultate especially the lung bases, noting
- the degree and symmetry of air entry
- any added sounds
In the context of reduced inspiratory capacity, augmenting inspiration with a positive pressure breathing device can assist auscultation further.
Respiratory Musculature
- to assess diaphragm function, palpate the degree and symmetry of upper abdominal rise during quiet and forced inspiration
- to assess breathing pattern, palpate the lower lateral aspect of the rib cage bilaterally and confirm any signs of paradoxical breathing during inspiration
- to assess for increased work of breathing, palpate and confirm any excessive accessory muscle activity ie. scalenes, sternocleidomastoid, upper trapezius during quiet inspiration or speech
- to confirm high level SCI or potential for spinal nerve root injury, note any absence or weakening of accessory muscles recruitment that should occur during forced inspiration and expiration ie. scalenes, sternocleidomastoid, upper trapezius, pectorals. Specific muscle tests around the head and neck may not be appropriate in the acute phase but can be performed later.
Lung Volumes
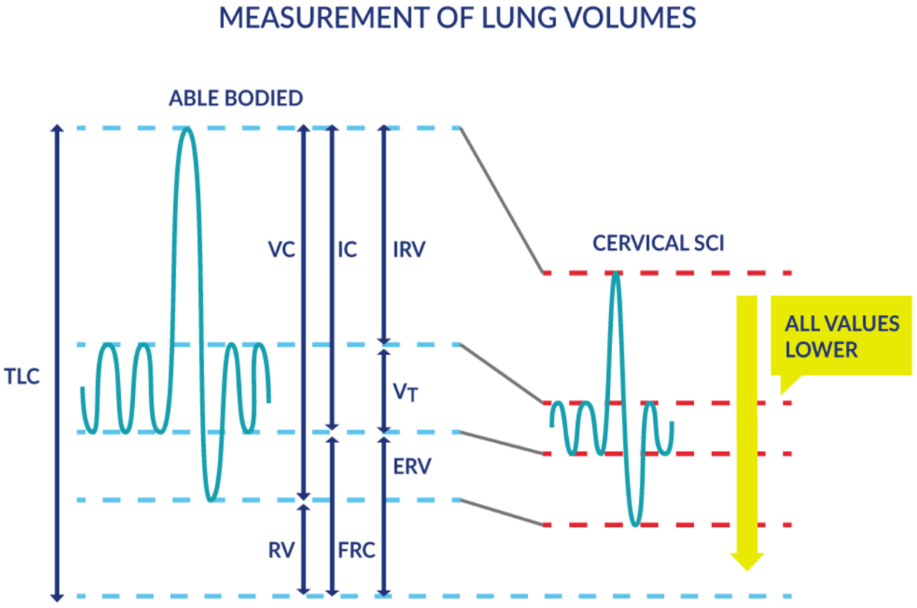
Changes to lung volume and functional respiratory capacity after SCI depends on the level and completeness of injury.
Respiratory function tests (RFTs) will establish a baseline to monitor for signs of deterioration or improvement.
RFTs can be completed via an endotracheal tube, tracheostomy or mouthpiece and should initially be completed in supine (no abdominal binder).
Seated spirometry is recommended when the individual is deemed medically stable and able to tolerate sitting for early rehabilitation. Capturing spirometry values in sitting with the addition of the abdominal binder can be utilised for education purposes.
A SCI which results in respiratory function changes induces a restrictive lung volume pattern.
In spirometry, this is characterised by no change to the FEV1 / FVC ratio because both values are reduced due to significant respiratory muscle paralysis. TLC is <80% predicted and FVC can be reduced to 20-60% of normal predictive values in acute cervical injuries and 80-90% in acute thoracic injuries.
However, an individual may have pre-existing obstructive lung disease denoted by FEV1 /FVC ratio <0.7.
Hence, following a SCI for an individual with pre-existing COPD, spirometry may yield a mixed pattern of restriction and obstruction. Regardless, establishing an individual’s RFT baseline is what is most important for ongoing monitoring.
Explanation of lung volumes and capacities: Lung Volumes and Capacities – YouTube
Source: Sheel AW, Welch JF, Townson AF (2018). Respiratory Management Following Spinal Cord Injury. In: Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Noonan VK, Loh E, Sproule S, McIntyre A, Querée M, editors. Spinal Cord Injury Rehabilitation Evidence. Version 6.0. Vancouver: p. 1-72. Microsoft Word – FINAL Resp V6 Chapter May 30 2018.docx (scireproject.com)
RFTs that can be easily performed with more clinically available devices are
- FEV1: Forced Expiratory Volume in 1 second
- FVC: Forced Vital Capacity
- PCF: Peak Cough Flow
Other indicative respiratory muscle assessments may be completed when the individual is more medically stable and may require more specialised equipment or environments are
- respiratory muscle strength assessment:
- MIP (Maximal Inspiratory Pressure): measures strength of diaphragm and other inspiratory muscles, along with compliance of lung/chest wall
- MEP (Maximal Expiratory Pressure): measures strength of abdominal and other expiratory muscles
- SNIP (Sniff Nasal Inspiratory Pressure): measures strength of diaphragm and other inspiratory muscles along with oesophageal pressure
Where no respiratory function testing equipment is available, the use of a timed sustained phonation can give some indication of lung volume and be used as a simple assessment of lung volume recruitment interventions. After a large inhalation, vowel /a/ pronounced with pitch and loudness of voice set at a natural level, can provide some indication of breath volume impairment.
Normal adult sustained phonation length ranges from 15-35seconds, with males typically achieving longer phonation time.
For more information on spirometry training: Queensland Health Spirometry Training Program – Metro North Health
Medical Investigations
An array of medical investigations can be utilised to diagnose any secondary complications that can arise from impaired respiratory dysfunction:
- Blood tests for arterial blood gas analysis as well as screening for infection and electrolytes
- Chest X-rays
- Computed Tomography Pulmonary Angiogram (CTPA): primarily for diagnosis of pulmonary embolism
- Diaphragm scanning: Ultrasound will diagnose whether the diaphragm is functioning but not provide detail on how well it is functioning, nor is it a useful tool for monitoring improvements. Assessing lung volumes will be effective for ongoing assessment.
References
Berlowitz DJ, Wadsworth B, Ross J. Respiratory problems and management in people with spinal cord injury. Breathe 2016; 12: 328–340.
Caruso P, Albuquerque AL, Santana PV, Cardenas LZ, Ferreira JG, Prina E, Trevizan PF, Pereira MC, Iamonti V, Pletsch R, Macchione MC, Carvalho CR. (2015) Diagnostic methods to assess inspiratory and expiratory muscle strength. J Bras Pneumol. Mar-Apr;41(2):110-23. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4428848/
Johansson, K., Seiger, Å., Forsén, M., Holmgren Nilsson, J., Hartelius, L. and Schalling, E. (2018), Assessment of voice, speech and communication changes associated with cervical spinal cord injury. International Journal of Language & Communication Disorders, 53: 761- 775. https://doi.org/10.1111/1460-6984.12380
Respiratory Management in Spinal Cord Injury – Physiopedia (physio-pedia.com)
Sheel AW, Welch JF, Townson AF (2018). Respiratory Management Following Spinal Cord Injury. In: Eng JJ, Teasell RW, Miller WC, Wolfe DL, Townson AF, Hsieh JTC, Connolly SJ, Noonan VK, Loh E, Sproule S, McIntyre A, Querée M, editors. Spinal Cord Injury Rehabilitation Evidence. Version 6.0. Vancouver: p. 1-72. Microsoft Word – FINAL Resp V6 Chapter May 30 2018.docx (scireproject.com)
Thoracic Key Chapter 16 Spinal Cord Injury Harris, K. and Ward, T. https://thoracickey.com/spinal-cord-injury/